28 Feb Pulmonary Ultrasound
Pleural effusion, Pulmonary Edema
Indications:
Respiratory distress, hypoxia, tachypnea
Probe Choice:
Curvilinear probe or phase array, although linear probe good for visualizing pleural pathology/lung sliding
Basic Views & Anatomy:
For pulmonary edema you can utilize a combination of anterior/lateral/posterior thoracic views, but it needs to be compared bilaterally.
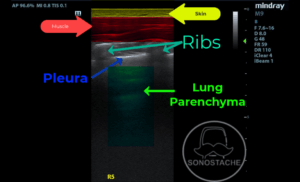
Here we can see a typical thoracic view with a linear probe. From the top down we see: 1) skin 2) muscle 3) ribs – round, hyperechoic structures with dark shadowing posteriorly 4) pleural line – hyperechoic linear structure that typically slides or crawls like “ants on a log” with normal respirations 5) lung parenchyma
Here is a curvilinear probe showing a normal thoracic view. It showcases normal pleural sliding & rib shadowing. Note the cardiac activity seen in the bottom right field, which is not an uncommon normal finding in pulmonary ultrasound.
For pleural effusion, a lateral view at the level of the diaphragm should be used (similar to a RUQ/LUQ from the FAST exam). Above we see gray curtain coming across the diaphragm, without obvious anechoic fluid collection.
For pneumothorax, often times in a supine patient the anterior chest views are best.
Pathology:
Pleural Effusion:
In the lateral view of the chest (similar to a LUQ FAST view) we see the diaphragm (curved bright white line) and cranial to that (left on the clip) we see anechoic fluid. This is the pleural effusion. We also see some atelectatic lung in the far left field.
Spine Sign:
In the far field we see the hyperechoic ridging of the spine. In pleural effusion it is called the spine sign when you see this continuing up into the thorax. Typically the air-filled parenchyma obscures the spine from being visualized, hence why you can see it with the anechoic pleural effusion.
Pulmonary Edema:
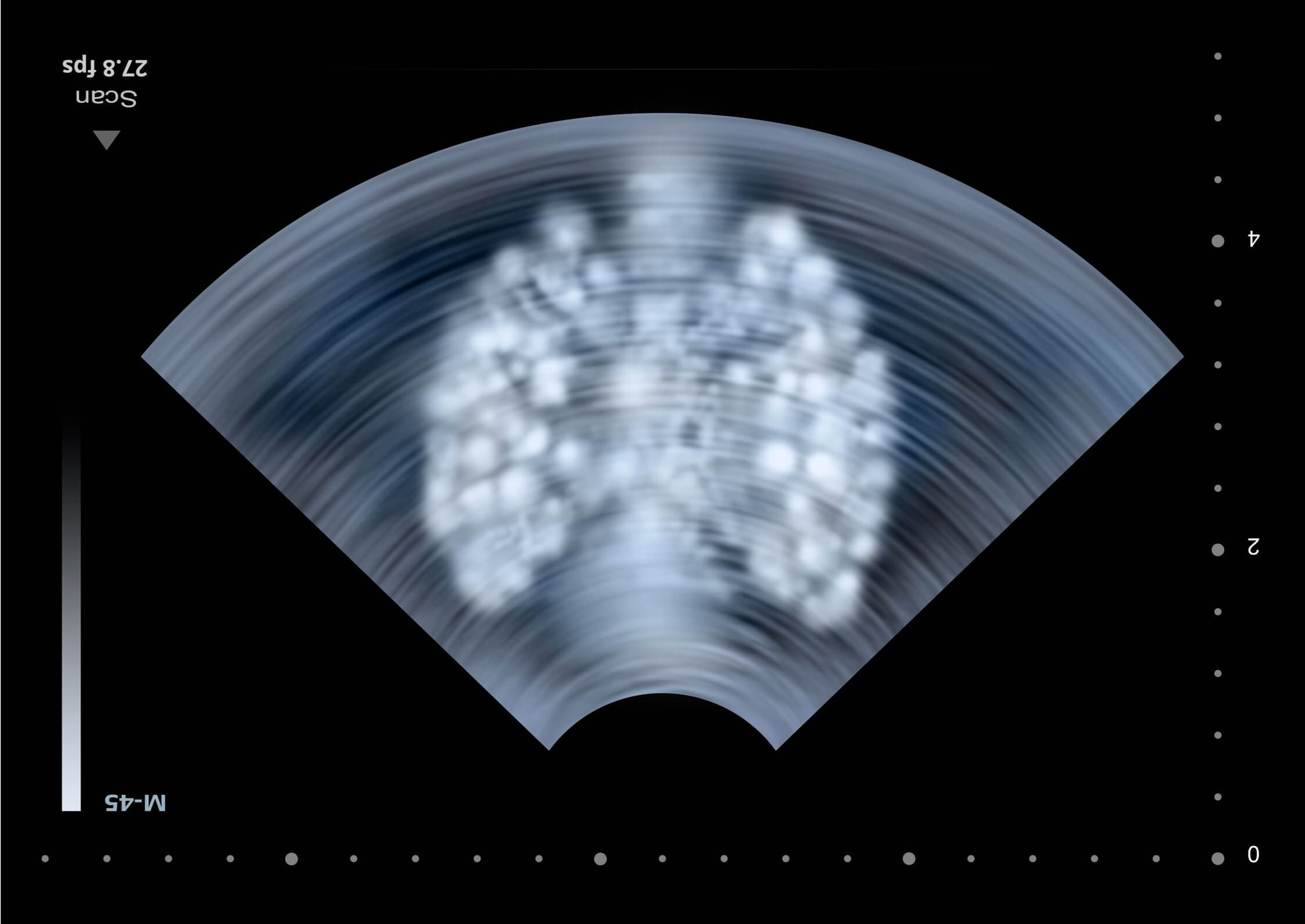
Here we see an artifact called B lines. These B lines are hyperechoic, extend from the pleura vertically, move with the pleura, and extend into the far field. These are most commonly associated with a build up of fluid in the lung tissue. However, these can be seen in other chronic conditions like pulmonary fibrosis, lung scarring from old infections, or septations of the lung. For this reason if you see 3 or more B lines in a single lung field, it is diagnostic.
B lines can be seen in a variety of conditions like ARDS, pulmonary contusion, viral and bacterial pneumonia. However, it is most likely going to be associated with pulmonary edema, especially if it is seen in multiple lung fields.
Here we see numerous B lines, coalescing into “confluent” B lines.
Pneumothorax:
Here we see the pleura (hyperechoic line) moving with respirations. This is called “lung sliding”.
Here we see no movement of the pleura, or absent lung sliding. This is indicative of pneumothorax. Of note, this can rarely be seen in other conditions with significantly decreased airflow in the pulmonary parenchyma like mainstem intubation, pulmonary blebs, pleurodesis.
Here we see a lung point, or a specific point where the pleura is not moving and transitions to a point where the pleura is moving. This is indicative of pneumothorax.
Artifacts:
A lines:
A lines are a reverberation artifact that can be seen in healthy lung. These are caused by ultrasound beams reflecting from the pleura and the ultrasound probe causing horizontal hyperechoic lines. These are always in incremental distance from the probe transducer to the pleura.
However, they can also be seen in cases of pneumothorax with a relative increase in the intensity of A-lines at the area of pneumothorax. However, there will not be lung sliding.
Here is a lung with pneumothorax and greater degree of A lines than that of the unaffected lung (with obvious lung sliding) in the same patient:
Mirror artifact:
Mirror artifact results from a highly reflective surface (like the diaphragm) and causes ultrasound beams to bounce between that surface and other structures at least once before returning to the ultrasound transducer. This produces a mirror image on the other side of the reflective surface.
Here we see a RUQ / lateral chest view with a mirror image artifact on the diaphragm producing what may look like a “second liver” in the far left field. This might be mistaken for pleural effusion or hemothorax.
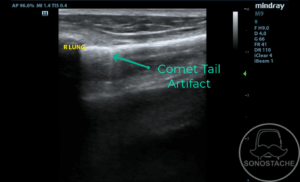
Comet Tail Artifact:
Comet tail artifacts can be encountered when evaluating the pleura. They are small reverberation artifacts that quickly fade through the depth of the image. They are not to be confused with B-lines, which pass from the pleura to the full depth of the image.
Pearls:
Depth should be 10-15cm for visualizing lung parenchyma (effusion or B lines)
A-lines present in normal lung
B-lines are abnormal, suggest fluid in lung
Remember to compare both lungs.
Pitfalls:
B-lines can be seen in conditions like fibrosis, ARDS, or asthma in addition to pulmonary edema. However, B-lines in standardized exams are most commonly associated with pulmonary edema.